This activity is provided by Med Learning Group.
This activity is supported by an educational grant from Regeneron Pharmaceuticals, Inc.
Copyright © 2019Med Learning Group. Built by Divigner. All Rights Reserved.
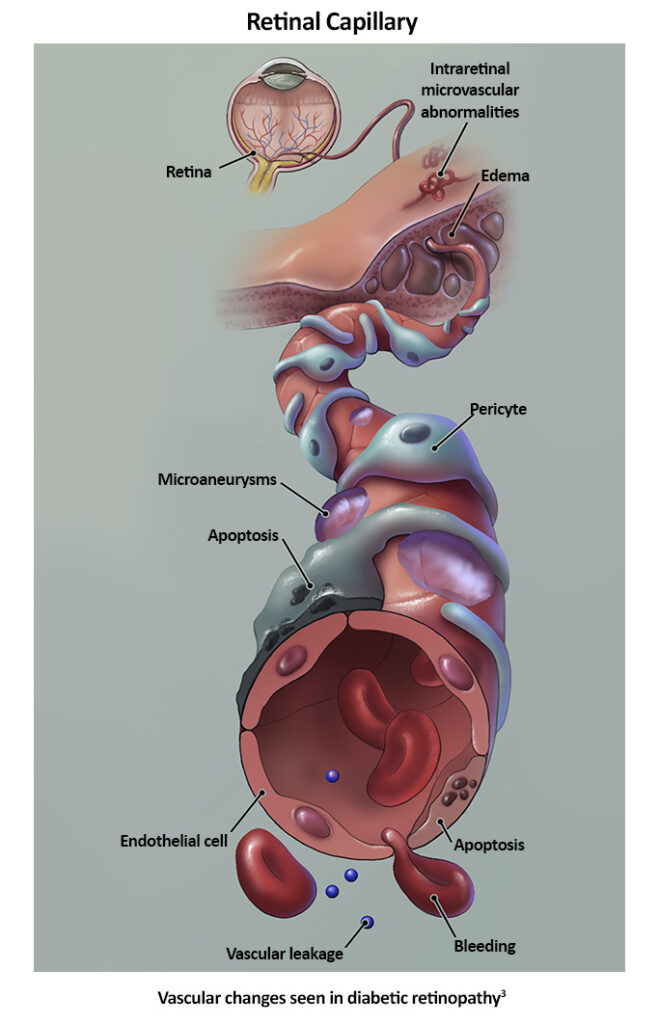
Chronic hyperglycemia from diabetes leads to tissue damage from various mechanisms.1 Microaneurysms are the earliest clinically evident stage of diabetic retinopathy; they result from advanced glycation-end products (AGEs) damaging basement membranes and other blood vessel wall components, including pericytes.1
Pericytes are cells within retinal capillary walls that provide physical strength and biochemical support to underlying endothelial cells.1 Damaging these cells weakens capillary endothelial cells, leading to localized outpouchings in capillary walls or microaneurysms.1 Microaneurysms (MAs) often rupture, causing hemorrhages in the deep retina, referred to as dot and blot hemorrhages on exam.1
Weakening of vessel wall integrity also leads to changes in vascular caliber, like in venous beading characterized by alternating areas of dilation and constriction of retinal veins.2 Intra-retinal microvascular abnormalities (IRMAs) are another example of blood vessel changes.4
Elevated levels of circulating glucose also result in oxidative stress and increased inflammatory factors, like protein kinase C (PKC), tumor necrosis factor-alpha (TNF-α), interleukin 6 (IL-6), IL-8, and IL-1.1,5 This activation of pro-inflammatory compounds leads to leukostasis and leukocyte adhesion, which are driving factors of capillary occlusion, especially when combined with endothelial damage.1 Cotton-wool spots (CWS) are visible signs of infarction of the retinal nerve fiber layer due to capillary occlusion.1
As capillary occlusion worsens, retinal ischemia occurs, leading to endothelial cell and neuroglial cell injury.1 Loss of neural retina cells results in inner retinal thinning.1 Retinal ischemia or hypoxia also triggers the upregulation of neovascular factors, like vascular endothelial growth factor (VEGF).1 VEGF has several effects, including elevating local inflammatory factors, angiogenesis, and increasing vascular permeability and local inflammatory infiltrates.1
Vascular permeability and breakdown of the blood-retina barrier increase over time with DR due to chronic inflammation and vascular damage, eventually leading to fluid leakage into the retina.1, 5 When the fluid buildup occurs in the macula, termed diabetic macula edema (DME), it can cause significant central vision impairment.1
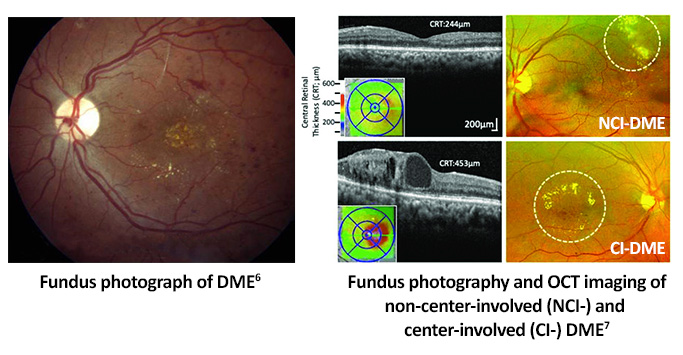
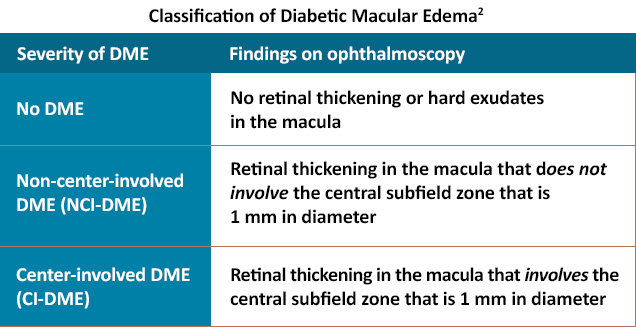
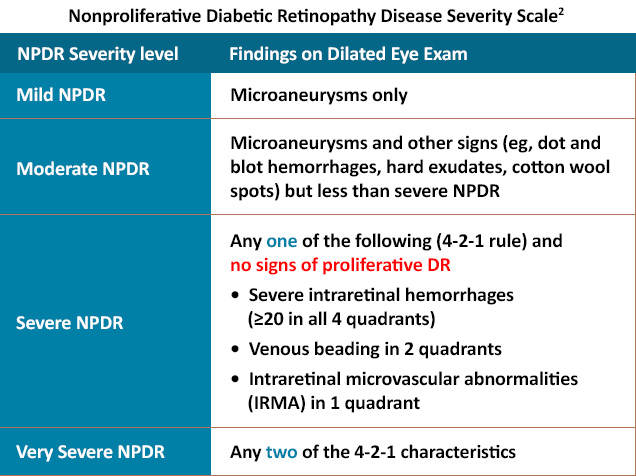
In general, diabetic retinopathy initially presents with nonproliferative abnormalities, like MAs and dot and blot hemorrhages. As the disease worsens, fundus exam findings may include cotton-wool spots, hard exudates, venous beading, and IRMAs.1 DME can occur at any time, with severity potentially following an independent course to other NPDR findings.2
This activity is provided by Med Learning Group.
This activity is supported by an educational grant from Regeneron Pharmaceuticals, Inc.
Copyright © 2019Med Learning Group. Built by Divigner. All Rights Reserved.
James P. Gills Professor of Ophthalmology
Professor of Ophthalmology, Johns Hopkins University School of Medicine
Wilmer Eye Institute, Johns Hopkins Medicine
Baltimore, MD

Specializing in Diabetes Eye Care & Education, Chous Eye Care Associates
Adjunct Professor of Optometry, Western University of Health Sciences
AOA Representative, National Diabetes Education Program
Tacoma, WA

Chief of Optometry, Sepulveda VA Medical Center
Professor, Southern California College of Optometry at Marshall B. Ketchum University
Sepulveda, CA
Ophthalmologist-in-Chief
Wills Eye Hospital
Philadelphia, PA

Director, Retina Research
Wills Eye Hospital
Professor and Chair of the Department of Ophthalmology
Thomas Jefferson University Hospitals
Philadelphia, PA

Director of Research, Retina Consultants of Houston
Associate Professor of Clinical Ophthalmology
Blanton Eye Institute & Houston Methodist Hospital
Houston, TX
The RELIEF Clinical Toolkit is an online tool that aims to provide clinicians with up-to-date information on the presentation, prognosis, pathophysiology, and treatment strategies for diabetic retinopathy (DR) in patients with diabetes who have or are at risk for developing DR. Click on one of the options below to learn more about DR.
This activity is provided by Med Learning Group.
This activity is supported by an educational grant from Regeneron Pharmaceuticals, Inc.
